Monkeypox has been declared a public health emergency of international concern (PHEIC) by the World Health Organization (WHO), the highest alert level previously only granted to COVID-19, Polio, the Ebola outbreak of 2014, and the Zika virus outbreak of 2015 to 2016.
“We have an outbreak that has spread around the world rapidly, through new modes of transmission, about which we understand too little, and which meets the criteria in the international health regulations. For these reasons, I have decided that the global monkeypox outbreak represents a public health emergency of international concern,” WHO Director General Tedros Adhanom Ghebreyesus told journalists on July 24.
Despite concluding that Monkeypox did not qualify as a PHEIC a month earlier, an evenly split vote at the second International Health Regulations Emergency Committee meeting on July 21 resulted in the declaration of an emergency.
MORE ON MONKEYPOX
- New York City’s Monkeypox Vaccine Website Crashes Due to High Traffic Immediately Following Launch
- The Internet Hivemind Wants ‘Zero Monkeypox’ Policy Installed
- Wuhan Institute Created a PCR Test for Monkeypox in February: Chinese Scientific Journal
The decision was made after cases increased from 3,000 from 47 countries on June 25 to over 16,000 cases from 75 countries by July 23.
Tedros added, “WHO’s assessment is that the risk of Monkeypox is moderate globally and in all regions, except in the European region where we assess the risk as high. There is also a clear risk of further international spread, although the risk of interference with international traffic remains low for the moment.”
Hardest hit areas
Success
You are now signed up for our newsletter
Success
Check your email to complete sign up
There were 3,591 confirmed Monkeypox cases by July 26 in the United States, with the most cases in New York, California, and Illinois, with 900, 356, and 350 cases, respectively, according to the U.S. Centers for Disease Control and Prevention (CDC).
There were 19,188 confirmed cases worldwide in 76 countries, 70 of which have not historically reported Monkeypox. Spain had the most cases at 3,738, followed by the U.S. in second, the United Kingdom with 2,432 cases in third, Germany with 2,410 cases in fourth, and France with 1,567 cases in fifth.
Previously, Monkeypox had broken out in the U.S. in April of 2003 when a shipment of approximately 800 small mammals, including six types of rodents, was imported from Ghana to Texas. Specifically, testing by the CDC revealed that “two African giant pouched rats, nine dormice, and three rope squirrels were infected with monkeypox virus.”
Prairie dogs near where the animals were housed became infected, and subsequently spread the disease to people. Touching sick animals, receiving bites or scratches that broke the skin, and cleaning the cages or beddings of sick animals were activities associated with increased risk of infection.
Transmission and severity
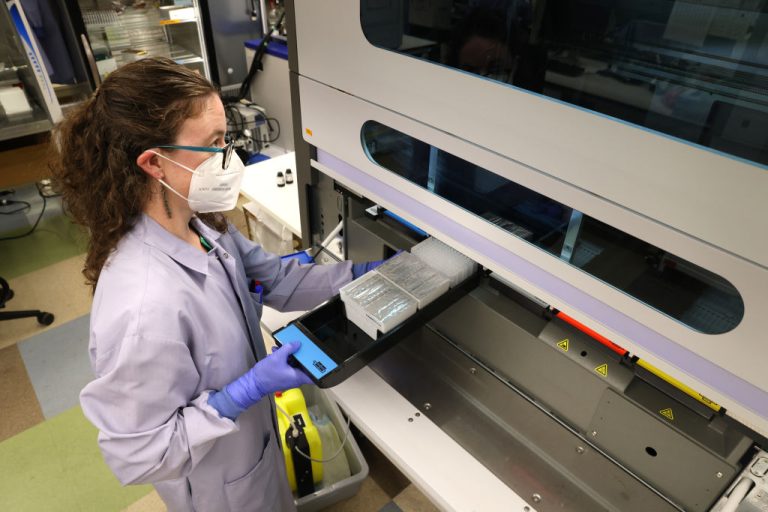
The manifestations of the disease were analyzed in the largest study to date published in the New England Journal of Medicine on July 21, with data spanning from April 27 to June 24 at 43 sites in 16 countries.
The study showed among 528 polymerase-chain-reaction (PCR)-confirmed cases, “98% of the persons with infection were gay or bisexual men, 75% were White, and 41% had human immunodeficiency virus infection; the median age was 38 years.”
Transmission of the disease was likely mediated by sexual activity in 95 percent of affected persons. A rash was seen in 95 percent of cases, with 64 percent having less than 10 lesions.
73 percent had anogenital lesions, and 41 percent had mucosal lesions in the mouth, throat, conjunctivae, and anus. Common systemic symptoms were “fever (62%), lethargy (41%), myalgia (31%), and headache (27%),” with other coincident sexually transmitted infections found in 109 of 377 persons (29 percent) tested.
The incubation period, or time between exposure and manifestation of symptoms, was a median of 7 days, but ranged between 3 and 20 days. The most common medical settings of presentation were Human Immunodeficiency Virus (HIV) clinic, sexual health clinic, and the emergency department, accounting for 29 percent, 23 percent, and 20 percent of cases, respectively.
Most of the cases were mild, with 13 percent of cases admitted to the hospital and no reported serious complications. Pain and bacterial superinfection were common reasons for admission, however, the study stated, “Rare serious complications (myocarditis and epiglottitis) were observed, and therefore the full spectrum of the disease and complications needs further study.”
According to John Thornhill, a consultant physician in sexual health and HIV and author of the study, “It is important to stress that monkeypox is not a sexually transmitted infection in the traditional sense; it can be acquired through any kind of close physical contact. However, our work suggests that most transmissions so far have been related to sexual activity—mainly, but not exclusively, among men who have sex with men.”