According to a study, published in the Journal of Clinical Investigation by the Northwestern University Feinberg School of Medicine, a secondary bacterial infection of the lung (pneumonia) was “extremely common in patients with COVID-19,” and by applying machine learning to medical record data scientists found that “secondary bacterial pneumonia, that does not resolve, was a key driver of death in patients with COVID-19.”
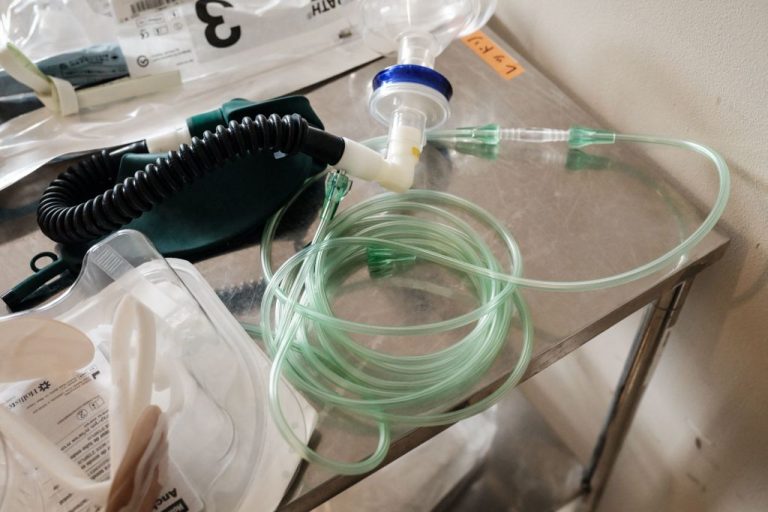
The analysis suggests that patients who required a mechanical ventilator also developed a secondary infection, an infection that was responsible for a higher mortality rate than the COVID-19 infection, meaning the cure may have been more deadly than the disease.
“Our study highlights the importance of preventing, looking for, and aggressively treating secondary bacterial pneumonia in critically ill patients with severe pneumonia, including those with COVID-19,” Benjamin Singer, a pulmonologist at Northwestern University in Illinois wrote.
The researchers examined the records of 585 people admitted to intensive care at the Northwestern Memorial Hospital in Illinois who all had severe pneumonia and/or respiratory failure, 190 of which also had COVID-19.
Researchers also discovered that nearly half of patients with COVID-19 developed a secondary infection due to the use of a ventilator.
Success
You are now signed up for our newsletter
Success
Check your email to complete sign up
“Those who were cured of their secondary pneumonia were likely to live, while those whose pneumonia did not resolve were more likely to die,” Singer wrote, adding that, “Our data suggested that the mortality related to the virus itself is relatively low, but other things that happen during the ICU stay, like secondary bacterial pneumonia, offset that.”
The researchers concluded that “Bacterial infections may even exceed death rates from the viral infection itself,” and that the evidence revealed that “COVID-19 does not cause a ‘cytokine storm,’ that was often believed to be the cause of death in COVID-19 patients.
A “cytokine storm” is believed to be the overwhelming inflammation that drives organ failure in one’s lungs, kidneys, brain and other organs in COVID-19 patients.
The findings of the machine learning technique employed, dubbed “CarpeDiem,” refutes the cytokine storm theory as there was no evidence of multi-organ failure in any of the patients studied, however they did develop ventilator-associated pneumonia (VAP).
READ MORE:
- Excess CO2 Exposure From Mask Mandates Behind Spike in Stillbirths, Posits Peer Reviewed Study
- US to Lift vaccine Mandate for Foreign Entries and Government Workers
- IBM Freezes Hiring on Positions Such as Human Resources, Looking to Replace Them With AI
Caution required
Scientists cautioned that a patient’s need for a ventilator, that leads to a secondary infection, does not imply that a COVID-19 infection is less dangerous only that “The relatively long length of stay among patients with COVID-19 is primarily due to prolonged respiratory failure, placing them at higher risk of VAP.”
The findings highlight a need for further study and also show how machine learning can reveal patterns in data that may not be immediately recognized by researchers.
The scientists say that the next step in the research will be to use “molecular data from the study samples and integrate it with machine learning approaches to understand why some patients go on to be cured of pneumonia and some don’t.”
They hope to expand the technique to larger datasets and use the model to make predictions that can be used to improve outcomes for critically ill patients.
Catherine Gao, also a pulmonologist at Northwestern said that “The application of machine learning and artificial intelligence to clinical data can be used to develop better ways to treat diseases like COVID-19 and to assist ICU physicians managing these patients.”