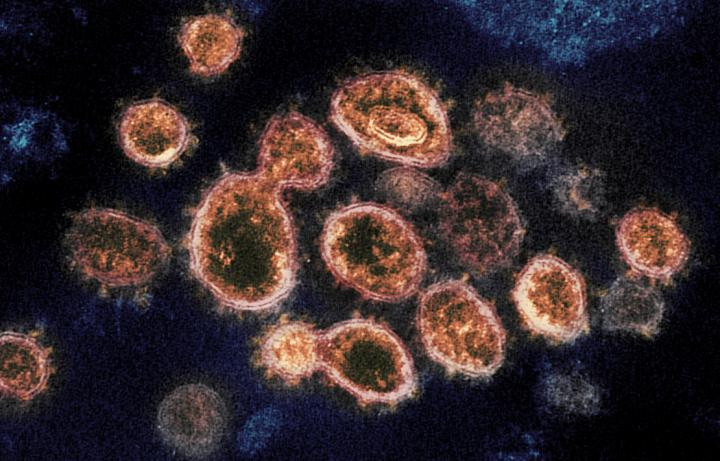
A recent study published by two Chinese scientists working for a university in Sweden has found evidence that the full length spike protein of SARS-CoV-2, the novel coronavirus that causes Coronavirus Disease 2019 (COVID-19), damages a crucial DNA repair mechanism involved in the human body’s adaptive immunity.
The study, titled SARS–CoV–2 Spike Impairs DNA Damage Repair and Inhibits V(D)J Recombination In Vitro was authored by Hui Jiang and Ya-Fang Mei of the Department of Clinical Microbiology, Virology at Umea University in Sweden and published in the scientific journal Viruses on Oct. 13 after first being submitted on Aug. 20.
The Abstract states, “Clinical studies have indicated that patients with severe COVID–19 exhibit delayed and weak adaptive immune responses,” and that the mechanism SARS-CoV-2 uses to impede adaptive immunity was currently unclear.
Jiang and Mei note this topic is of critical interest because, “Adaptive immunity plays a crucial role in fighting against SARS–CoV–2 infection and directly influences the clinical outcomes of patients.”
Adaptive immunity
A textbook on human biology found on the University of Minnesota’s website describes the significance of the human body’s adaptive immunity function, noting it takes effect “after exposure to an antigen either from a pathogen or a vaccination.”
Success
You are now signed up for our newsletter
Success
Check your email to complete sign up
While adaptive immunity takes significantly longer than the innate immune system to become established, it has the virtue of being highly specificized to the invading pathogen.
The text uses two examples to explain antigen exposure, “An antigen is a small, specific molecule on a particular pathogen that stimulates a response in the immune system. One example of an antigen is a specific sequence of 8 amino acids in a protein found only in an influenza virus, the virus responsible for causing ‘the flu.’”
“Another example is a short chain of carbohydrates found on the cell wall of Neisseria meningitidis, the bacteria that causes meningitis.”
READ MORE:
- Experiment Finds Pfizer Vaccine Desaturates and Clots Red Blood Cells, Contains ‘Garbage’ Crystalline Structures and Fibers Under Microscopy
- Fired Whistleblower in Phase 3 Pfizer COVID Vaccine Clinical Trial Study Location Says Data was Falsified
- FDA Approved Oral Anti-Blood Clot Drug for Children Just Months Before Youth Vaccine Rollout
It goes on to explain the specifics of how the adaptive immune system generates B and T cell lymphocytes to combat an invader, “In adaptive immunity, activated T and B cells whose surface binding sites are specific to the antigen molecules on a pathogen greatly increase in numbers and attack the invading pathogen.”
“Their attack can kill pathogens directly or they can secrete antibodies that enhance the phagocytosis of pathogens and disrupt the infection. Adaptive immunity also involves a memory to give the host long-term protection from reinfection with the same type of pathogen carrying the same antigens; on reexposure, this host memory will facilitate a rapid and powerful response.”
V(D)J recombination
The Swedish study states definitively in its Abstract, “Here, by using an in vitro cell line, we report that the SARS–CoV–2 spike protein significantly inhibits DNA damage repair, which is required for effective V(D)J recombination in adaptive immunity.”
“Mechanistically, we found that the spike protein localizes in the nucleus and inhibits DNA damage repair by impeding key DNA repair protein BRCA1 and 53BP1 recruitment to the damage site.”
The authors do not shy away from the implication their finding may have on today’s messenger RNA and adenovirus vector vaccines, “Our findings reveal a potential molecular mechanism by which the spike protein might impede adaptive immunity and underscore the potential side effects of full-length spike-based vaccines.”
In a Jan. 31 article published in the journal Microbiology Spectrum titled V(D)J Recombination: Mechanism, Errors, and Fidelity, the function is explained as an intricate method utilized by the human immune system to craft the antigen-binding receptors of T cells through the rearrangement of DNA, “The exons encoding the antigen-binding domains are assembled from so-called V (variable), D (diversity), and J (joining) gene segments by ‘cut and paste’ DNA rearrangements.”
“This process, termed V(D)J recombination, chooses a pair of segments, introduces double-strand breaks adjacent to each segment, deletes (or, in selected cases, inverts) the intervening DNA, and ligates the segments together.”
“Diversity is tremendously amplified by the characteristic variability at the junctions (loss or gain of small numbers of nucleotides) between the various segments. This process leverages a relatively small investment in germline coding capacity into an almost limitless repertoire of potential antigen-binding specificities.”
The article describes this function as an “elegant process,” but cautions its fine and exact nature carries with it substantial potential for disaster, “A system that must break chromosomal DNA several times in order to generate a functional antigen receptor gene—many millions of times over the lifetime of an organism—creates significant opportunities for error.”
“The necessity of enforcing a high degree of fidelity in V(D)J recombination has been recognized for decades. Aberrant V(D)J recombination events do occur, and they can be life-threatening…”
COVID’s immune system impact
The Umea study summarizes several clinical studies in order to illustrate the effect the virus has on the adaptive immune system, “SARS–CoV–2 infection extraordinarily affects lymphocyte number and function. Compared with mild and moderate survivors, patients with severe COVID–19 manifest a significantly lower number of total T cells, helper T cells, and suppressor T cells.”
“Additionally, COVID–19 delays IgG and IgM levels after symptom onset. Collectively, these clinical observations suggest that SARS–CoV–2 affects the adaptive immune system. However, the mechanism by which SARS–CoV–2 suppresses adaptive immunity remains unclear.”
It further explains that the DNA repair system and immune systems are not only “the primary systems that higher organisms rely on for defense against diverse threats and tissue homeostasis,” but that cutting-edge science has shown “these two systems are interdependent, especially during lymphocyte development and maturation.”
The authors state that a loss of function in crucial DNA repair proteins have been found to “inhibit the production of functional B and T cells, leading to immunodeficiency.”
This point is critical to the topic of defending public health against the pandemic because, “In contrast, viral infection usually induces DNA damage via different mechanisms…If DNA damage cannot be properly repaired, it will contribute to the amplification of viral infection-induced pathology.”
“Therefore, we aimed to investigate whether SARS–CoV–2 proteins hijack the DNA damage repair system, thereby affecting adaptive immunity in vitro.”
Full-length vaccine spikes
The authors preface their Results section by stating, “DNA damage repair occurs mainly in the nucleus to ensure genome stability,” but points out that with SARS-CoV-2, its proteins generated during infection are synthesized in the cytostol (liquid matrix inside a cell).
The duo constructed “viral protein expression plasmids together with spike and nucleoprotein expression plasmids,” finding results consistent with multiple other studies that discovered “proteins are indeed localized in the nucleus, and nucleoproteins are mainly localized in the cytosol.”
However, the study quietly noted, “Surprisingly, we found the abundance of the spike protein in the nucleus.”
The researchers begin to tie this key point into how DNA damage repair is inhibited, “Because spike proteins are critical for mediating viral entry into host cells and are the focus of most vaccine strategies, we further investigated the role of spike proteins in DNA damage repair and its associated V(D)J recombination.”
“In the native state, spike proteins exist as inactive full–length proteins,” the authors state, noting that host cell proteases cleave the spike into subunits during the process of its entering the cell at the time of infection.
This point was important because several different testing methodologies used in the study found that “Only the full–length spike protein strongly inhibited” two different kinds of DNA repair mechanisms, generating the definitive conclusion that “the spike protein directly affects DNA repair in the nucleus.”
Another array of tests concurrently determined that “SARS–CoV–2 full–length spike protein inhibits DNA damage repair by hindering DNA repair protein recruitment.”
This finding is significant to the public because, as the authors note, “Many approved SARS–CoV–2 vaccines, such as mRNA vaccines and adenovirus–COVID–19 vaccines, have been developed based on the full–length spike protein.”
Today’s novel gene therapy vaccines are substantially different from classical inactivated virus vaccines. While the latter uses a neutered variant of the whole pathogen to expose the immune system and elicit a response, the former does not use any pathogen at all, instead relying on a messenger RNA genetic instruction (Moderna, Pfizer-BioNTech) or a double-stranded DNA genetic instruction delivered in a vector of an adenovirus (AstraZeneca, Johnson & Johnson) to force human cells to grow the SARS-CoV-2 spike protein in an attempt to cause an immune system response.
The authors then tested whether the spike protein inhibited V(D)J recombination, “For this, we designed an in vitro V(D)J recombination reporter system according to a previous study,” and found that “Compared with the empty vector, spike protein overexpression inhibited RAG–mediated V(D)J recombination in this in vitro reporter system.”
“…Our data provide[s] valuable details on the involvement of spike protein subunits in DNA damage repair, indicating that full–length spike–based vaccines may inhibit the recombination of V(D)J in B cells, which is also consistent with a recent study that a full–length spike–based vaccine induced lower antibody titers compared to the RBD–based vaccine.”
In the Discussion section of the paper, the authors are conclusive about the impact the virus has on the immune system, “Our findings provide evidence of the spike protein hijacking the DNA damage repair machinery and adaptive immune machinery in vitro.”
“Although no evidence has been published that SARS–CoV–2 can infect thymocytes or bone marrow lymphoid cells, our in vitro V(D)J reporter assay shows that the spike protein intensely impeded V(D)J recombination.”
Finally, the duo posited a theory as to why COVID-19 is hitting the elderly harder, “This may be because SARS–CoV–2 spike proteins can weaken the DNA repair system of older people and consequently impede V(D)J recombination and adaptive immunity.”