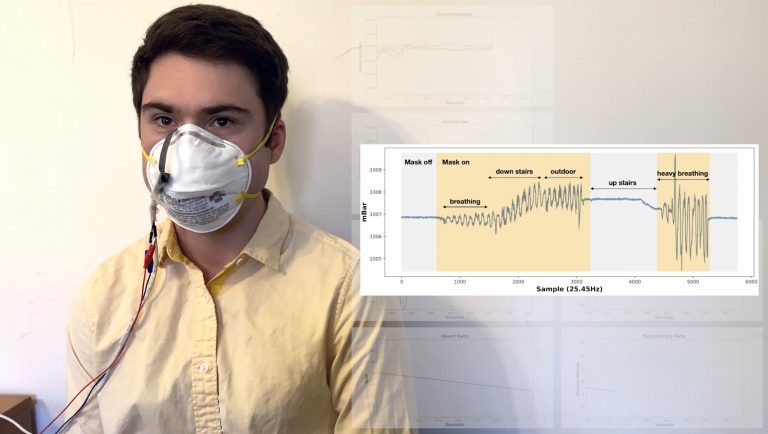
Researchers have developed a smart sensor that can be applied to masks that monitors a user’s breath rate, heart rate, and other health metrics—but fails to address essential factors relevant in the Coronavirus Disease 2019 (COVID-19) pandemic climate, such as oxygen deprivation or efficacy against viruses.
“We wanted to design an intelligent face mask for health care professionals that does not need to be inconveniently plugged in during the middle of a shift,” the research head Josiah Hester, an Assistant Professor, said in a Northwestern University press release.
READ MORE:
- Canadian Hospital Allegedly Denies 7-Year-Old Boy Treatment for Broken Arm Over Medical Mask Exemption
- Delta CEO Wants AG Garland and the DOJ to Place Anti-maskers on No-Fly List
- Speech Therapist Notices a 364 Percent Soar in Child Patients After Mask Mandates
The “FaceBit,” as the invention has been catchily-dubbed, is a relatively bulky chip to dangle on your face at the size of a quarter. The device attaches using a magnet to any mask, specifically professional-grade N95, KF94, or the lower-standard Chinese-made KN95 respirators.
Self-powered
The battery derives part of its energy supply from movements taken by its user. The rest comes from sunlight and the warmth of the user’s breath, and is promoted as having a runtime of at least 11 days before needing to be plugged in.
Success
You are now signed up for our newsletter
Success
Check your email to complete sign up
“We augmented the battery’s energy with energy harvesting from various sources, which means that you can wear the mask for a week or two without having to charge or replace the battery,” the Assistant Professor said.
But even if you manage to keep your battery running for two weeks, manufacturers’ guidelines nonetheless prescribe that N95 respirators be replaced after three to four hours weartime, at a maximum, according to a September article by KSL News Radio. So you must refit your device regularly, anyhow.
“If you wear a mask for 12 hours or longer, sometimes your face can become numb,” Hester continued, in an apparent disregard of sanitary masking guidelines.
Monitoring and feedback
“You might not even realize that your mask is loose because you cannot feel it, or you are too burnt out to notice,” Hester continued. “We can approximate the fit-testing process by measuring mask resistance. If we see a sudden dip in resistance, that indicates a leak has formed, and we can alert the wearer.”
The sensor communicates via Bluetooth connection with the user’s mobile phone through a custom app that processes several metrics. One feature of the product is that it can alert when the user’s heart rate is unstable, or if mask fit develops a leak.
“Your heart is pushing a lot of blood through the body, and the ballistic force is quite strong,” Hester explains. “We were able to sense that force as the blood travels up a major artery to the face.”
Omissions
The device does not offer any explanation as to why the user would have a heightened heart rate.
The announcement also didn’t touch upon major health issues that can occur with protracted mask or medical respirator usage, such as carbon dioxide saturation and oxygen deficiency of the blood, syndromes that can occur in as little as seconds after the user applies his mask.
According to Hester, FaceBit offers an initial step toward practical on-face sensing and inference. Hester also enthusiastically lauded the apparatus for it being a “sustainable,” “convenient,” and “comfortable” monitoring instrument for frontline workers and others.
“I’m really excited to hand this off to the research community to see what they can do with it,” he added.
What the gadget further doesn’t serve to study is the degree to which masks can deliver on what they are purported to do by government and corporate mandates, namely, to diminish virus-containing aerosols—if at all—simply because the instrument was not built with a sensor capable of detecting pathogens, let alone measuring them.